- Visibility 147 Views
- Downloads 18 Downloads
- DOI 10.18231/j.ijce.2024.040
-
CrossMark
- Citation
Exploring maxillary molar root morphology: A case of extra palatal canal
Introduction
Dental caries is among the most common chronic diseases.[1] If not treated promptly, it can advance to infect the pulp and, eventually, the periapical tissues, resulting in irreversible pulpitis or apical periodontitis. Root canal therapy is the preferred treatment in such cases, aimed at eliminating bacteria and diseased tissue from the pulp and periapical area, and replacing them with a biocompatible material. Studies by Siqueira JF et al., and Lin LM et al. suggest that complex root anatomy is a leading factor in endodontic treatment failure. The shape and structure of pulp canals can vary significantly among individuals, even within the same racial group. Therefore, understanding root canal anatomy is critical for successful endodontic treatment.
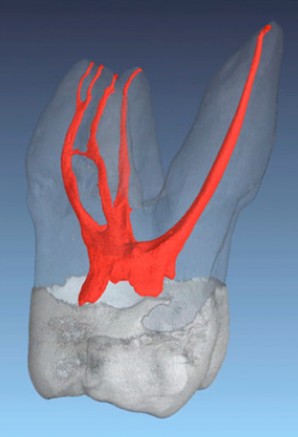
Anatomic characteristics of permanent maxillary molars are generally described as a group of teeth with 3 roots, 1 palatal and 2 buccal, each root having 1 root canal (Figure 1). However, the literature describes wide variations in root canal morphology of maxillary first molars. Cleghorn et al., did a comprehensive review of the root and root canal morphology of the maxillary first molar. Cleghorn et al., reported the incidence of two canals in the mesiobuccal root as 56.8% and of one canal was 43.1% in a weighted average of all reported studies.[2]
The occurrence of extra palatal canal in a maxillary molar with MB2 has been very rarely reported. This case report presents, management of an extra palatal canal in a maxillary first molar with MB2.
Case Report
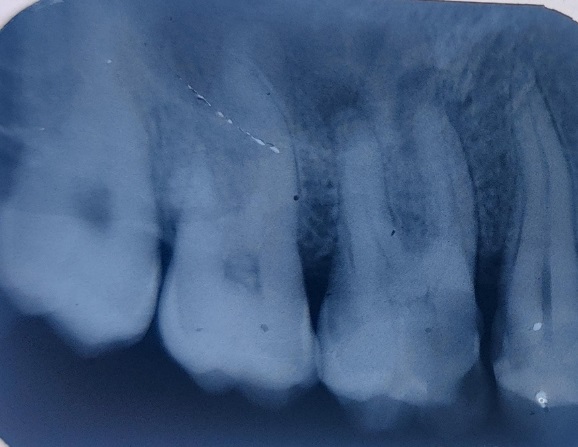
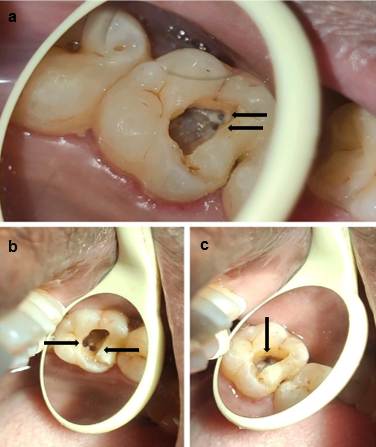
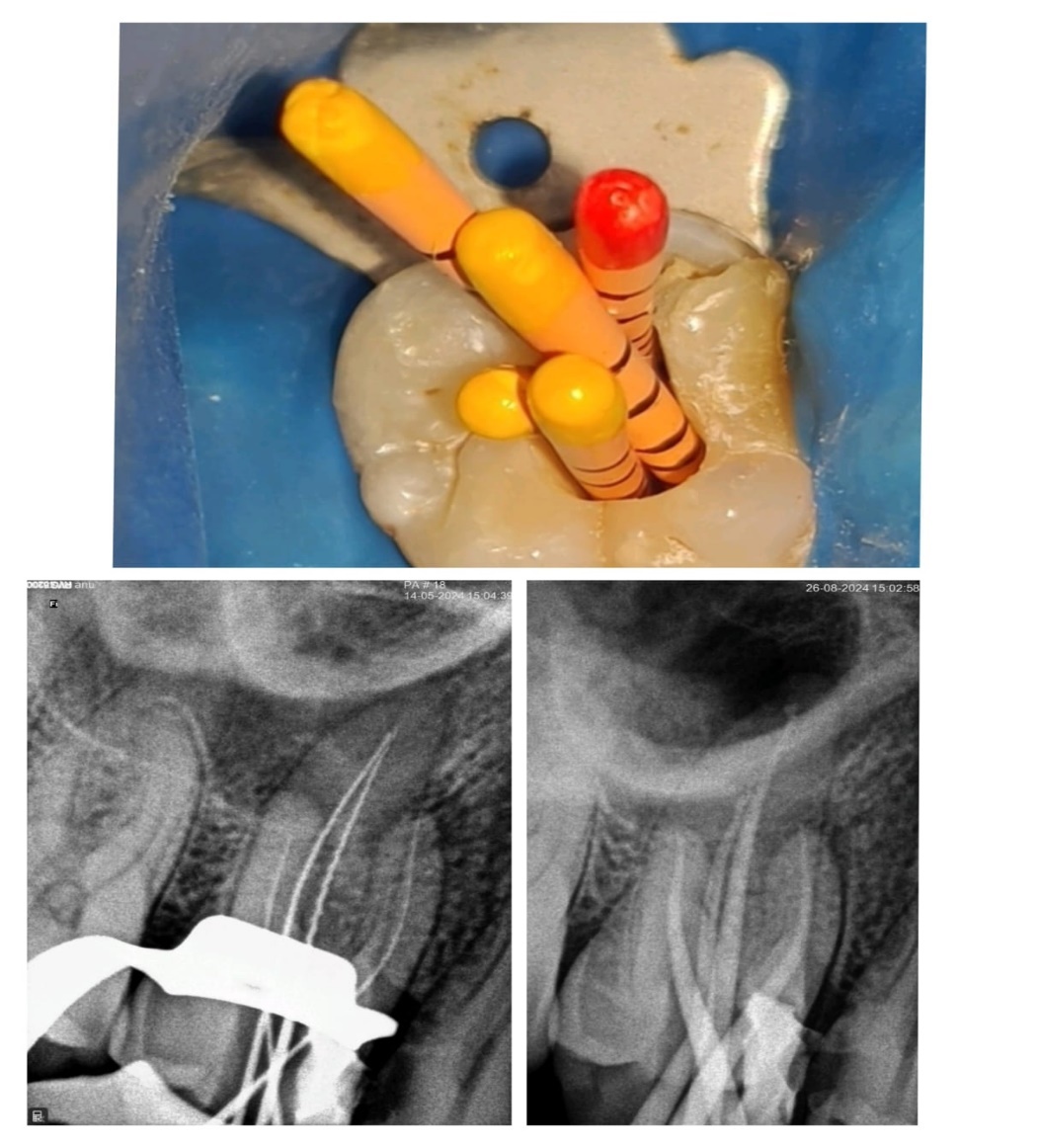
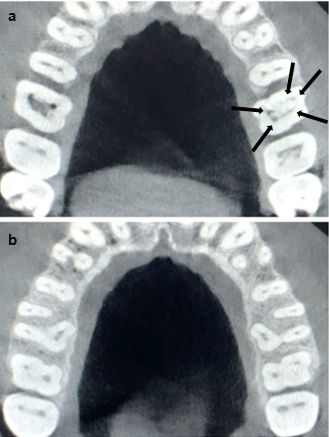
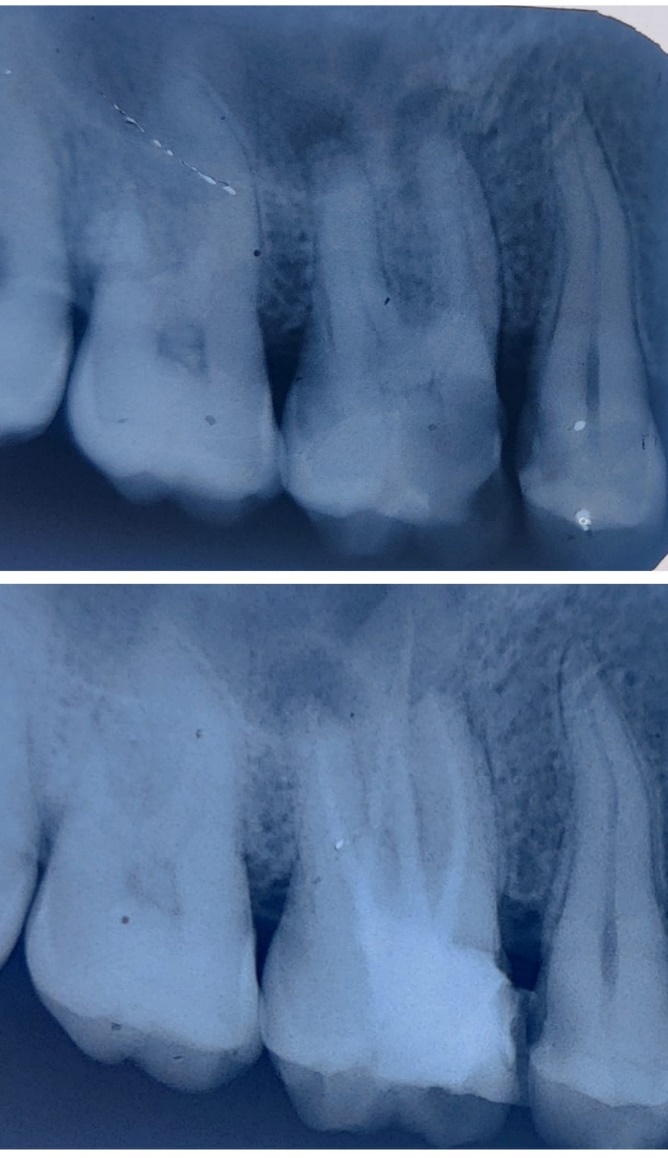
A 35-year-old male patient was referred to Department of Endodontics, Kamineni Institute of Dental Sciences and presented with continuous pain in relation to right maxillary first molar(16). Clinically, Intraoral examination showed, a deep carious lesion in relation to 16, with positive percussion test. Radiographic examination (periapical radiograph) revealed a periapical radiolucency associated with mesial and distal roots of 16 ([Figure 2]). Cold test and electric pulp sensitivity tests showed negative response implying non-vital pulp. A diagnosis of pulpal necrosis with acute peri-apical abscess was made, and endodontic treatment was planned. Local anaesthesia was administered. Pre-endodontic build up was done using composite to close mesial class-II cavity, Access cavity preparation was done ([Figure 3]a, b and c), and canals were located, including an extra-palatal canal (disto-palatal), with the aid of an endodontic microscope. The working length was determined using an apex locator and confirmed radiographically. During radiographic examination for working length determination, mb2 was faintly visible ([Figure 4]). Due to the unclear canal morphology, a CBCT scan was requested. The CBCT scan revealed ([Figure 5]a, b):
The presence of four distinct root canals in the maxillary right first molar: two in the mesio-buccal root (MB1 and MB2), one in the distobuccal root, and an additional accessory canal in the palatal root.
The MB2 canal was positioned slightly mesio-palatal to MB1 and extended toward the apex.
The extra-palatal canal was located distal to the main canal, indicating a bifurcation at the coronal third of the palatal root, which was merging apically.
The MB2 canal was thoroughly negotiated under microscope. Irrigation with sodium hypochlorite, EDTA, and saline was used to clean and disinfect all canals, including the challenging extra-palatal and MB2 canals. Calcium hydroxide was placed as an intracanal medicament for one week to ensure complete disinfection. At the follow-up appointment, the canals were obturated using gutta-percha with bio-ceramic sealer, followed by a coronal seal with composite resin. A final radiograph confirmed the successful obturation of all canals ([Figure 6]).
Discussion
Managing an extra-palatal canal and an MB2 canal in a maxillary first molar presents unique challenges in endodontics, requiring thorough understanding of the tooth's anatomy, meticulous techniques, and advanced tools. These additional canals are not uncommon but are often overlooked due to their complexity and variable occurrence.
Maxillary first molar anatomy
The maxillary first molar typically has three roots: mesiobuccal, distobuccal, and palatal, each generally containing a single canal. However, anatomic studies show that the mesiobuccal root often contains two canals (MB1 and MB2), and occasionally an extra canal may be found in the palatal root.
MB2 Canal in the Mesiobuccal Root
The mesiobuccal root is particularly prone to variations. The MB2 canal is present in approximately **60-90%** of maxillary first molars, but it is often missed during conventional root canal treatment.[3] The MB2 canal is typically smaller and more difficult to locate due to its variable position and angulation, necessitating advanced techniques such as enhanced magnification and adjunctive diagnostic tools like cone-beam computed tomography (CBCT). [4] MB2 canals often exhibit complex morphology. They may either remain separate or merge with the MB1 canal before exiting the apex and failing to locate and treat the MB2 canal is a common cause of endodontic failure in maxillary molars. [5]
Extra-Palatal Canal
Although less common, the presence of an extra canal in the palatal root is documented in literature. Cleghorn et al., (2006) found that the palatal root usually contains one large canal, but variations such as bifurcation or the presence of a second canal can occur. Despite the rarity of extra-palatal canals compared to MB2 canals, their management demands careful exploration using CBCT and magnification, as these tools are critical for detecting and treating these less common configurations. [6]
Clinical case considerations
In a clinical case where both an extra-palatal canal and an MB2 canal are present, the following considerations are essential:
Diagnostic phase
Preoperative CBCT imaging is crucial for identifying additional canals that are not visible on conventional radiographs. CBCT allows for three-dimensional evaluation of the internal anatomy, enhancing the detection of extra canals. The use of dental microscopes for magnification significantly increases the likelihood of locating the MB2 canal, as well as other anatomically challenging canals. [4]
Access cavity modification
Traditional triangular access cavities may need modification to provide better visualization and access to additional canals. A trapezoidal access opening may be necessary when both MB2 and extra-palatal canals are present". [5] Clinicians must balance the need for improved access with the preservation of tooth structure, especially in cases involving multiple canals". [7]
Canal negotiation and instrumentation
The MB2 canal, once located, often exhibits a tortuous and narrow configuration, requiring careful negotiation with small hand files (e.g., #08 or #10 K-files), followed by rotary or reciprocating systems to enlarge the canals" (Schroeder et al., 2002). Similar cautious instrumentation is needed for the extra-palatal canal, if present, due to its typically narrow size" [2]. The foramen of the buccal canals were enlarged to medium (#35) and palatine canal to large (#45). [8] Irrigation with sodium hypochlorite and EDTA are recommended to ensure proper debridement of the complex anatomy in these canals". [5]
Obturation
Thermoplasticized gutta-percha or warm vertical compaction techniques are often preferred to ensure proper filling of intricate canal systems involving MB2 or extra-palatal canals. [5] Adaptation of obturation materials is crucial in preventing endodontic failure in cases involving multiple canals. [7]
Prognosis and follow-up
"Endodontic cases involving extra canals, particularly MB2 and extra-palatal canals, may be at higher risk of failure if these canals are not thoroughly cleaned, shaped, and obturated. Long-term success depends on the precision of treatment. Studies show that clinical success rates in maxillary molar root canal therapy improve when extra canals are identified and managed correctly" (Schroeder et al., 2002; Ng et al., 2011).
Conclusion
This case report highlights the importance of careful diagnostic evaluation and thorough knowledge of root canal anatomy variations, such as extra-palatal canal in maxillary first molar with mesio-buccal canal-2 (MB2). The successful management of this case was facilitated using imaging techniques, magnification, and precise instrumentation, underscoring the need for a meticulous approach in similar complex cases. Clinicians should remain vigilant for anatomical variations to ensure comprehensive cleaning, shaping, and obturation, improving the prognosis for endodontic treatments.
Source of Funding
None.
Conflict of Interest
None.
References
- R H Selwitz, A I Ismail, N B Pitts. Dental Caries. Lancet 2007. [Google Scholar]
- BM Cleghorn, WH Christie, CC Dong. Root and root canal morphology of the human permanent maxillary first molar: a literature review. J Endod 2006. [Google Scholar]
- FS Weine, HJ Healey, H Gerstein, L Evanson. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surg Oral Med Oral Pathol 1969. [Google Scholar]
- B Karabucak, E Buonocore, F C Setzer. Microscope-enhanced endodontic diagnosis and treatment planning: A review. J Endod 2016. [Google Scholar]
- FJ Vertucci. Root canal morphology and its relationship to endodontic procedures. Endod Top 2005. [Google Scholar]
- BM Cleghorn, WH Christie, CC Dong. The root and root canal morphology of the human mandibular second premolar: a literature review. J Endod 2006. [Google Scholar]
- YL Ng, V Mann, K Gulabivala. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J 2011. [Google Scholar]
- R S Signori, L M Klassmann. MB2 in Maxillary Molars: Location and Alternatives for Treatment. Biomedical J Sci Tech Res 2019. [Google Scholar]
- Introduction
- Case Report
- Discussion
- Maxillary first molar anatomy
- MB2 Canal in the Mesiobuccal Root
- Extra-Palatal Canal
- Clinical case considerations
- Diagnostic phase
- Access cavity modification
- Canal negotiation and instrumentation
- Obturation
- Prognosis and follow-up
- Conclusion
- Source of Funding
- Conflict of Interest
